ECG Case 132
Thank you to my colleague Dr Danny Marhaba for submitting this case for discussion
A 57-year-old man is referred in by his GP following two weeks of episodic left axillary pain. HR 73, BP 134/64, SpO2 97 RA.
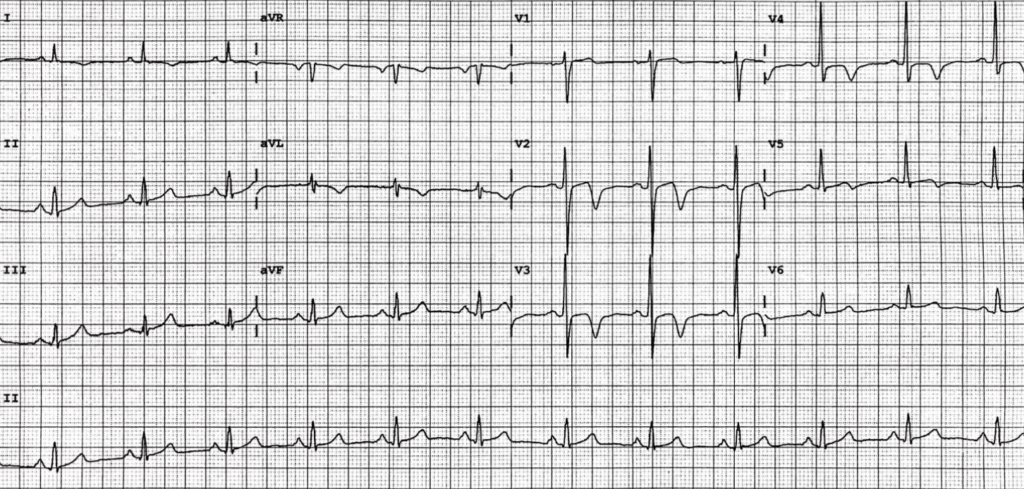
He is pain free at triage when the following ECG is taken:
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
- Normal sinus rhythm, rate 72 bpm
- Deeply T-wave inversion in V2-4, without significant ST segment changes
- R wave progression is preserved (R wave in V3 > 3mm)
We recall from ECG Case 123 that our differentials for right precordial T-wave inversion in patients with symptoms of acute coronary syndrome (ACS) include:
- Ischaemia (including Wellens Syndrome)
- Posterior myocardial infarction
- Right ventricular strain (including pulmonary embolism)
- Hypertrophic cardiomyopathy (especially apical type) — with high mid-anterior QRS voltages
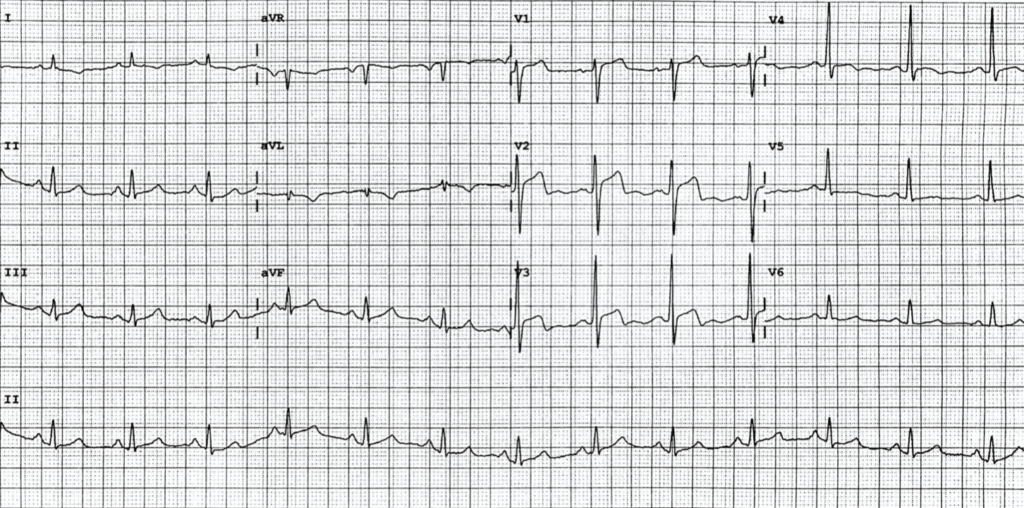
Whilst working through your above differentials, our patient has a further episode of chest pain. ECGs are captured at the time of pain and also following self-resolution:
t + 8 minutes (recurrence of pain)
What is your interpretation?
Reveal answer
- There is “pseudonormalisation” of previously inverted T-waves in V2-4
- ST segment elevation is seen in V2-3 – straightening of this segment creates the appearance of wide, bulky T waves which we recall are suggestive of evolving infarction (remember, it is the area under the T wave that is more important than the overall height)
t + 17 minutes (pain resolved)
What is your interpretation?
Reveal answer
- Changes are similar to our initial ECG, with return of deep T-wave inversion in leads V2-4
OUTCOME
Such dynamic T-wave changes in V2-4 suggests this is indeed Wellens syndrome. “Pseudonormalisation” in our second ECG represents evolving infarction (as opposed to ischaemia) – given recurrent episodes of chest pain in the department, this patient requires emergent intervention.
Urgent angiogram revealed severe diffuse left main coronary artery stenosis and severe mid LAD stenosis for which he underwent successful PCI. Initial troponin taken in the emergency department later returned a negative result.
CLINICAL PEARLS
Wellens Syndrome is a clinical syndrome characterised by a pattern of biphasic or deeply inverted T waves in V2-3, plus a history of recent chest pain that is not resolved. It is highly specific for critical stenosis of the left anterior descending artery (LAD). These patients usually require invasive therapy, do poorly with medical management, and may suffer MI or cardiac arrest if inappropriately stress tested.
“Pseudonormalisation” may mask all ischaemic changes
Although our second ECG above is concerning in itself due to anterior STE and HATW, such evolving infarction may not always be so evident. Pseudonormalisation of previously inverted T waves may manifest as a “normal” ECG. With self-resolution of chest pain, serial troponins in these patients are often negative. If only one ECG is taken on arrival with the occurrence of pain, the diagnosis of Wellens syndrome may be missed. It sounds simple, but Wellens syndrome underpins the importance of all patients presenting pre-hospital and to emergency departments undergoing serial ECGs, especially with changes in pain.
Understanding T wave changes
![Evolution of T-wave inversion [A-D] after coronary reperfusion in STEMI reperfusion and in Wellens syndrome (NSTEMI)](https://litfl.com/wp-content/uploads/2018/08/Evolution-of-T-wave-inversion-A-D-after-coronary-reperfusion-in-STEMI-reperfusion-and-in-Wellens-syndrome-NSTEMI-1024x352.png)
Patients with Wellens Syndrome present with one of two ECG patterns:
- 75% will have a pattern of deeply inverted T waves in leads V2-3 (type B)
- 25% will demonstrate a biphasic T wave with negative terminal portion (type A). These type A changes can be subtle and are more often overlooked.
In patients with Wellens, a sudden complete occlusion of the LAD causes a transient anterior MI, manifesting as either “pseudonormalised” anterior T waves or an anterior STEMI. Reperfusion of the LAD (e.g. due to spontaneous clot lysis) causes resolution of ST segment changes, and T waves become biphasic or inverted. The T wave morphology is identical to patients who reperfuse after a successful PCI.
Note that this sequence of events is not limited to anterior leads – similar changes may be seen in inferior or lateral leads, e.g. with RCA or circumflex occlusion.
Differentials for right precordial T wave inversion
In patients presenting with chest pain and ECG features in V2-3 suggestive of Wellens Syndrome, we must always consider and examine for changes suggestive of pulmonary embolism. As seen in ECG Case 123, associated T-wave inversion in leads V1 and III is highly specific for the diagnosis of PE. In addition, ECG changes will usually not be dynamic with recurrence of pain.
- “Pseudonormalisation” of T waves may mask all ischaemic changes in Wellens Syndrome. Serial ECGs are of the utmost importance in detecting this condition that requires prompt intervention
- Whilst most commonly seen in critical LAD stenosis, the T wave morphology of Wellens Syndrome can be seen in inferior and/or lateral leads due to RCA or LCx stenosis
- Examine leads III and V1 closely for associated T-wave inversion that suggests RV strain due to PE
Further reading
Related topics
Expert Review
- Smith SW. If you had recorded an ECG during chest pain, what would it have shown?. Dr Smith’s ECG Blog. 2018 June
TOP 150 ECG Series
MBBS (UWA) CCPU (RCE, Biliary, DVT, E-FAST, AAA) Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Editor-in-chief of the LITFL ECG Library. Twitter: @rob_buttner
Interventional cardiologist, ECG and hemodynamics fan. MD, Assoc. Prof. at Marmara University, Pendik T&R Hospital, Assoc. Editor at Archives of TSC, ESC National Prevention Coordinator




thanks for this awesome explanation!!