Five years ago Mark Horowitz seemed an unlikely skeptic of psycho-pharmaceuticals. He had been taking the popular antidepressant Lexapro virtually every day for 15 years. He was so fascinated by the drugs that he spent three years hunched over a dish of human brain cells in a laboratory at King's College London, measuring the effect of human stress hormones and drugs like Prozac and Zoloft.
Then, when he tried to wean himself off the medication, he suffered panic attacks, sleep disruptions and a depression so debilitating that he had to move back to his parents' house in Australia—symptoms that he says were far worse than anything he experienced prior to going on the drugs. He went online and found thousands of others in a similar pickle. They had been unable to kick one of the psychiatric drugs known as Selective Serotonin Reuptake Inhibitors, or SSRIs, which include Lexapro, Zoloft and Prozac, among others. Since withdrawal symptoms were thought to be mild and temporary, many of them, like him, had been told by doctors that they were experiencing a relapse of their depression.
The experience galvanized Horowitz to dig deeper into the claims that pharmaceutical companies, and the scientists they fund, have been making about these popular antidepressants.
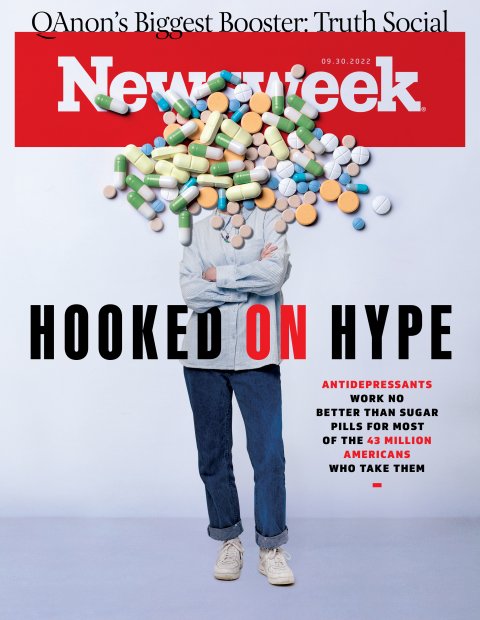
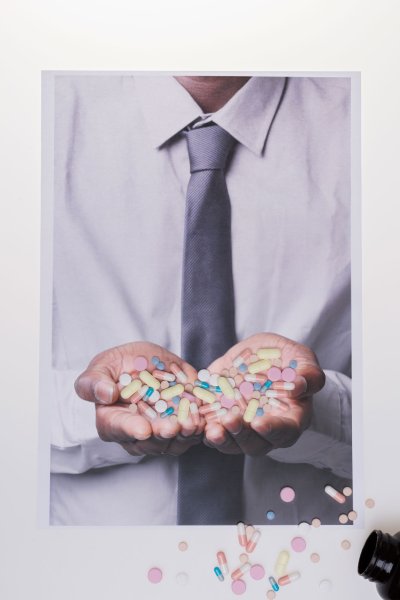
Hailed as a revolution for the treatment of depression when they first came out in the 1980s, SSRIs have become a mainstay of mental health treatment. Family doctors with little psychiatric training now prescribe them for adults and children alike. In 2019, one in eight Americans—43 million in all—were taking an SSRI, and those numbers have likely risen among a public ridden with COVID-induced anxiety. During the pandemic, doctors phoned in so many new prescriptions for Zoloft, the FDA warned of a drug shortage.
Evidence is mounting, however, that doctors are vastly overprescribing SSRIs. Although there is widespread agreement that SSRIs help some people with severe depression, these patients are a small minority of people who take the drugs. Only about 15 percent derive any more benefit from the drugs than they would a sugar pill, one recent study found. In addition, withdrawal symptoms for long-term users may be more severe that previously thought—sometimes worse than the original disorder. According to the Centers for Disease Control and Prevention, more than 60 percent of Americans on SSRIs—almost 26 million people—have been taking the drugs for more than two years and six million have been on them for a decade or more. Some patients may stay on SSRIs simply to avoid withdrawal symptoms, say some experts.
"People do get better on the drug—but in the vast majority of cases it's not because of what's in the drug," says Irving Kirsch, associate director of the Program in Placebo Studies and the Therapeutic Encounter at Beth Israel Deaconess Medical Center and Harvard Medical School. "There are other treatments that are at least equally effective, and that don't carry the risks."
The issue has cleaved the psychiatric community. Some clinicians and researchers are calling for a new approach to the treatment of depression that includes curtailing the use of SSRIs. Others, including the drug companies, insist that the drugs save lives and worry that attention-getting studies casting doubt on the effectiveness of SSRIs could end up discouraging the very people who need them most and who could be helped by them.
This tension ratcheted up considerably in July, with the publication of a provocative new study that has captured the attention of the mainstream media and millions of Americans taking the drugs and sent ripples of anxiety through the psychiatric profession.



Viral Science
One of the authors of the new study is Horowitz, now a research scientist at University College London. His July paper, "The serotonin theory of depression: a systematic umbrella review of the evidence," is aimed squarely at debunking the basis upon which pharmaceutical companies marketed drugs like Prozac, Lexapro and Zoloft to consumers for decades: namely, the idea that depression is associated with deficits in the concentrations or activity of the brain chemical serotonin.
The pharmaceutical industry used that idea to market the drugs to consumers for many years, and it remains a kind of shorthand some doctors use to explain to their patients how the drugs work. As a result, according to the study's authors, between 85 and 90 percent of the public believe that low serotonin levels cause depression. After reviewing data from previous studies involving hundreds of thousands of individuals, Horowitz and his colleagues concluded that there is little to no evidence that this is true.
"The drug companies convinced us that if you're sad, you should go to your doctor and seek treatment," Horowitz told Newsweek. "They've made us all believe that normal aspects of the human condition are a medical illness called major depressive disorder—that normal reactions to difficult situations are a chemical brain problem that needs a medical solution. They convinced people these are very 'mild' drugs that are very easy to stop. None of this is true."
This conclusion came as no surprise to the psychiatric establishment. Neuroscientists have known for years that depression is more than a simple imbalance in serotonin levels. But the paper hit a nerve with the general public. It generated more than 500 stories in the mainstream media, was shared on Twitter almost 7,000 times and was among the top 5 percent of the most widely shared scientific papers, according to Altimetric, a company that tracks public attention to research.
Horowitz and the paper's other co-authors have been using the attention to call for a fundamental reassessment of how mental illness is treated. "We have a mistaken view of what psychiatric drugs are doing," says Dr. Joanna Moncrieff, professor of Critical and Social Psychiatry at University College London. She is also Horowitz's boss and the lead author of the serotonin paper. "This idea that they work by targeting the underlying biological mechanisms that produce the symptoms of mental disorders is actually not supported by evidence for any type of mental disorder, whether that's depression or schizophrenia or whatever," she told Newsweek.
Instead, she argues, the drugs change "normal brain states" and "normal mental states and processes" in ways not that much different than recreational drugs like alcohol. They obscure psychotic symptoms by "superimposing" an abnormal drug state over other effects. In SSRIs, the small advantages seen in placebo-controlled trials, she suggests, can be attributed to emotional numbing that reduces the intensity of feelings causing the depression and anxiety, at the expense of a fuller experience of the ups and downs of life. The crippling sadness that sometimes follows a reduction in SSRI medication is caused by the chemical dependence the drugs can cause in the brain and withdrawal effects.
"It's not helpful to think of depression as a brain disease," she says. "I think that we should be thinking of it as an emotional reaction to life circumstances
and life events. And indeed, there is very strong evidence that people who suffer from adverse life events are much more likely to get depressed."
Most leading experts on the biology of depression would agree with that last point. In recent years, research studies have linked stress to depression. By one estimate, those who experience major depressive episodes are 2.5 times more likely to have experienced a stressful event, such as the death of a loved one, in the months leading up to the onset of the disease than those in a control group. Stress has been linked in other studies to a greater likelihood of treatment resistance, poorer outcomes and a higher rate of relapse.
Disagreements center on what the best treatment is. Moncrieff argues that psychotherapy aimed at improving coping skills is a safer and more effective solution than drugs. Many psychiatrists, conversely, argue that stress seems to cause actual physical changes in the brain, which medication can help to reverse.
Stress hormones cause the brain to be flooded with the neurotransmitter glutamate, placing it in a state of chronic overstimulation, says Dr. Michael Thase, a professor of psychiatry at UPenn's Perelman School of Medicine. "Glutamate is elevated when you are distressed and aroused—it's also elevated briefly when we're really enthusiastic and up about stuff," he says. "But the kind of elevation of glutamate that's associated with prolonged intractable, severe distress becomes neurotoxic."
Over time, brain imaging suggests, this overactivation can cause neurons to shrink and become less connected to one another. Tiny proteins, which support dynamic growth and a healthy brain, dry up in the neurons of the hippocampus, the memory center of the brain, and the prefrontal cortex, where executive functions reside. The spiny arms that form the connections between neurons, known as dendrites and axons, shrivel up. This toxic environment seems to cause a dysregulation of the brain systems needed to perform routine actions. A lack of sleep and an inability to function in daily life creates more stress, releasing more glutamate. The patient spirals downwards.
Something about SSRIs, many psychiatrists believe, seems to reverse this vicious cycle. Changing the dynamics of serotonin transmission is thought to be the first step in a complex "cascade of events" that seems to help the brain to heal, says Dr. Jerrold Rosenbaum, who served as psychiatrist-in-chief at Massachusetts General Hospital for many years, and is a leading authority on anxiety, depression and other mental disorders. This chain reaction induces a new state of "neuroplasticity," or mental flexibility, increasing the ability of neurons to form new connections to one another, even causing the brain to give birth to new neurons. "The increase in neuroplasticity is more consistent with the time course for SSRI response," he says. "This explains why they take a couple weeks to produce a response."
For some people, SSRIs can help restore the brain to a healthy state. But that doesn't mean the drugs should be used for months or years, as many doctors now prescribe them. "For first-time SSRI users, if it works substantially, you shouldn't take it for longer than six to nine months, unless you got really good reason to do that," says Thase. "You and your doctor [should] have worked out a plan of what to do after those six to nine months."
The 26 million Americans who have been on the drugs for two years or more may have questions for their doctors.


No Better Than a Sugar Pill
A few weeks after the Horowitz paper came out, a team of researchers at the U.S. Food and Drug Administration, along with Kirsch, a long-time critic of the drugs from Harvard Medical School, published the most comprehensive analysis to date of all the antidepressant clinical trial data in its files, much of it previously unpublished. The study, which examined 232 placebo-controlled trials of 73,388 patients diagnosed with major depressive disorder, suggested that the active ingredients in 10 of the most popularly prescribed antidepressant medications made a meaningful difference in only 15 percent of the patients who took them, almost always in those patients suffering from the most severe depression.
The study, along with others, adds to mounting evidence suggesting that the active ingredients of SSRIs can make the biggest difference in patients who have severe depression, and often are of only marginal utility to those suffering from mild to moderate depression. Why, then, are they so overprescribed?
One reason may be that SSRIs are effective for many people not because the drug
itself is working but because of the placebo effect. The simple act of treating a patient creates an expectation of healing that results in an improvement in the patient's condition. Previous research has generally found that the placebo effect is successful in 30 to 40 percent of cases of depression—in other words, a third of those who receive a pill or a shot that has no active ingredient get better from the simple fact that they are receiving care and attention from another human being.
The FDA study provides a glimpse of the true power of the SSRI placebo effect and the efforts of the pharmaceutical industry to use these effects to bolster the data on their own drugs.
To win approval for a new drug, FDA requires drug makers to submit the results from "two well-designed clinical trials" that demonstrate the drug itself is more potent than the placebo effect, "to be sure that the findings from the first trial are not the result of chance or bias." But the rules place no limit on how many clinical trials a drug company can conduct to get those two positive results. And though negative trial results must be registered with the FDA, there is no requirement that drug companies publish them.
As a result, the failure rate of trials of antidepressants is far higher than most people understand, says Dr. Erick Turner, a former FDA clinical reviewer, who is now a professor of psychiatry and pharmacology at Oregon Health and Science University. Dr. Turner, who was trained as a psychiatrist, recalls discovering multiple negative trials in the first psychotropic drug application he reviewed for the agency in the late 1990s, and being so shocked that he immediately took it to his boss.
"It happens all the time," he recalls his boss telling him, before revealing that roughly 40 percent of antidepressant trials, in his estimation, were negative or failed.
By 2015, Dr. Turner had left the agency for academia. He conducted a review of the publication status of 74 studies involving 12 antidepressant agents with 12,564 patients and found that the drugs beat the placebo in only 51 percent of the studies in the FDA files—an outcome that was not reflected in the published medical literature at the time. Of 33 studies that had negative or questionable results, 22 were never published and 11 were published in a way that falsely conveyed a positive outcome, wrote Dr. Turner in the New England Journal of Medicine. Even though half of the trial had failed, 94 percent of the published trials reported positive trial results. The full scope of this disconnect has only recently come into public view.
Harvard's Kirsch has been studying the little-understood, yet profoundly potent phenomenon of the placebo effect for decades. Over the years he has shown that a simple sugar pill can reduce pain and lower blood pressure and that the placebo effect can even improve treatment outcomes for knee surgery. He first began analyzing published data and attempting to quantify the effect on antidepressant trials in the late 1990s, and his conclusions, and blanket condemnation of SSRIs, have been controversial.
"These data indicate that virtually all of the variation in drug effect size was due to the placebo characteristics of the studies," he wrote in one paper. Kirsch has long argued that better, safer treatments with fewer side effects are available and SSRI use should be significantly curtailed.
Many of Kirsch's colleagues consider him a provocateur. But his latest paper is difficult to refute. Four out of five of Kirsch's co-authors work for the FDA, including Marc Stone, the agency's deputy director for safety. Kirsch says they enlisted him to collaborate on a groundbreaking review of the FDAs own files that was published in August. (The FDA declined to make Stone or his other collaborators available for this story).
The study of 232 placebo-controlled trials with 73,388 patients diagnosed with major depressive disorder found that while 88.5 percent of those taking the drugs saw some improvement in their depression symptoms, 84.4 percent in the placebo group did, too. The most significant differences only showed up when the researchers focused on patients that reported a large improvement, the kind most likely to be clinically relevant. These patients accounted for 24.5 percent of those taking the actual medication, compared to 9.6 percent of the placebo group—a difference of roughly 15 percent. "This confirms what I've been saying all along," says Kirsch.
That does not mean the mainstream psychiatric establishment is ready to embrace Kirsch's conclusion that SSRI use should be curtailed. Dr. Rosenbaum of Harvard suggests that the high placebo rates should not be taken to mean that SSRIs are not effective medications. The problem, he says, is that more than 40 years after the psychiatric profession created the category of major depression disorder, the definition of depression remains far too broad.
"You can have two people who don't have a single symptom in common and still meet the criteria" for depression, he says. "There are those with onset in childhood with depression, and others who don't develop it until late life. Some with brief and recurrent symptoms and some with chronic unremitting symptoms. Some episodes are influenced profoundly by external factors, and some seem completely autonomous."
As a result, he says, patients should consult with their doctors. It can be necessary for a patient to try five or six medications before finding the right one.
Dr. Andrea Cipriani, a professor of psychiatry at the University of Oxford in the United Kingdom, says that doctors treating conditions like cancer and cardiovascular disease have a multitude of options to choose from and can personalize treatments for patients. But the mental health field has yet to develop the diagnostic tools to do the same.
"We are still in the 19th century approach—we found a treatment, it should work for everybody," he says. "But that's not the case." Psychiatrists need to develop better methods that consider variables like severity, gender, number of previous episodes and genes when deciding which drugs to prescribe.
One way to improve results would be to distinguish between patients with severe depression, for whom SSRIs are most likely to be effective, from patients with less severe depression. But the diagnostic criteria doctors use may not be up to the task. In 2010, Dr. Jay Amsterdam, then director of a large mood disorder clinic at the University of Pennsylvania's Perelman School of Medicine, used his own questionnaire to measure severity among patients. For those with "very severe" depression, the results of SSRI medications were "markedly superior" to the placebo. For depressed patients with moderate symptoms, the drugs were no better than placebo.
Data on how often clinicians consider depression severity in prescribing SSRIs is not available. But in the early 2000s, researchers at Brown University reviewed the files of 147 patients treated at a local mental health care clinic. Although 40 percent of them had "mild" depression, doctors had prescribed antidepressants to 97 percent of patients.
Not-So-Mild Side Effects
Taking ssris is not free of risk. evidence has grown that SSRIs cause physical dependence and contribute to the kind of emotional numbing that Moncrieff describes.
Serotonin plays an important role in regulating the activity of other neurons and transmitters, often "calming them down," says Dr. Richard Shelton, a psychiatrist the University of Alabama at Birmingham and the founding director of the Depression and Suicide Research Center. This explains why a sudden spike in serotonin levels might help to counteract the effects of chronic and acute stress. While SSRIs can help with stress and anxiety, they don't do much to correct the loss of energy, interest and motivation that characterize depression. This is why many patients on SSRIs report an emotional dulling or numbing.
Withdrawal symptoms from SSRIs are also getting more attention. In the United Kingdom, where more than 17 percent of the adult population in England (7.3 million people) were prescribed antidepressants in 2017, policymakers have launched a broad assessment of who should take the drugs, and how often they should be prescribed.
In 2019, prompted in part by previous papers published by Horowitz on drug withdrawal, a British Parliamentary working group reviewed 24 studies examining the incidence, severity and duration of antidepressant withdrawal reactions. The goal was to assess the depression guidelines issued by the U.K.'s National Institute for Health and Care Excellence (NICE) and the American Psychiatric Association (APA), both of which stated that withdrawal reactions from antidepressants are "self-limiting," typically resolving in a week or two.
The researchers concluded that 56 percent of the people who came off antidepressants experienced withdrawal effects, nearly half of whom described them as "severe." Some reported that the effects lasted months—one patient reported symptoms lasting more than six years.
The results raise the prospect that many patients stay on SSRIs not so much for depression but to alleviate their withdrawal symptoms. "Since 2004, we've seen the average duration of time a person spends on these drugs more than double," says James Davies, a psychologist at the University of Roehampton, London, member of a parliamentary working group on prescription drug dependence and a co-author of the 2019 paper. "One of the arguments we make as to why that might be happening is because when people try to stop, they experience bad things and doctors reinstate the drugs as a consequence."
In response, late last year the U.K.'s NICE, an independent organization charged by the government with providing advice and guidance on health and social care, changed its depression guidelines, emphasizing patient choice, and recommending that antidepressant medications no longer be considered a first-line treatment for patients suffering from "less severe depression." Instead, it recommends that they choose from a menu of options that includes cognitive behavioral therapy (CBT), exercise, counseling or psychotherapy.
"There is now a wide acknowledgement in the U.K. that antidepressant withdrawal is a significant problem," says Davies. "A lot of people are out there suffering from severe and protracted withdrawal symptoms. They are in a lot of pain and we need to help them. That's the conversation we are having now in the U.K.—what can the government do?"
So far, no move has yet been made to change the clinical guidelines of the APA. (It declined to make a representative available for comment.) Neither has any such urgency caught on among the American psychiatric establishment. And even if it does, more expensive alternatives such as talk therapy may not be realistic for many people.
"When you start to move out to rural areas or inner city areas, access to these treatments is not really an option," says Dr. Rosenbaum. "So you have a choice to try something that is accessible, which is prescribing, or do nothing at all."
Joshua Gordon, Director of the U.S. National Institute of Mental Health (NIMH), notes that, since many Americans in mental distress lack access to qualified psychotherapists who take health insurance, most will go to their primary care doctor for care. And "the tools that are the primary care doctor's disposal are these safe, effective antidepressant medications."
"It would be great if we had better ones," he told Newsweek. "And yes, it would be great if we had wider access to alternative therapies, including psychotherapy, but they're certainly the safest and easiest to administer medications that we have. And they are effective."
In the meantime, the number of Americans taking the drugs is likely to continue to grow as a new generation of customers comes of age. Last fall, the American Academy of Pediatrics declared a national emergency in child and adolescent mental health. In December, the U.S. Surgeon General issued a mental health crisis advisory warning that from 2009 to 2019, the share of high school students who reported persistent feelings of sadness or hopelessness increased by 40 percent and encompassed more than 1 in 3 students. The pandemic, he suggested, has only made things worse.
Ever since beginning his calamitous effort to get off SSRIs, Horowitz has devoted himself to disproving the claims used to justify their widespread use, and lobbying lawmakers to take a second look. He now describes himself as no more neurotic than anyone in a Woody Allen movie and believes he should never have been prescribed SSRIs in the first place. And he is still weaning himself off the drugs. He now measures his daily dosage with an eye dropper.